What is Insomnia Disorder?
Insomnia Disorder is a chronic sleep disorder characterized by difficulty initiating or maintaining sleep, or both, despite adequate opportunities to sleep. This leads to impaired daytime functioning, distress, and reduced quality of life.
Symptoms:
- Difficulty falling asleep (onset insomnia)
- Waking up frequently during the night (middle insomnia)
- Waking up too early (terminal insomnia)
- Non-restorative sleep
- Daytime fatigue, mood disturbances, and difficulty concentrating
Types:
- Acute Insomnia (short-term, usually triggered by stress or events)
- Chronic Insomnia (long-term, lasting more than 3 months)
- Comorbid Insomnia (co-occurring with other medical or mental health conditions)
- Onset Insomnia (starts suddenly)
- Maintenance Insomnia (persists over time)
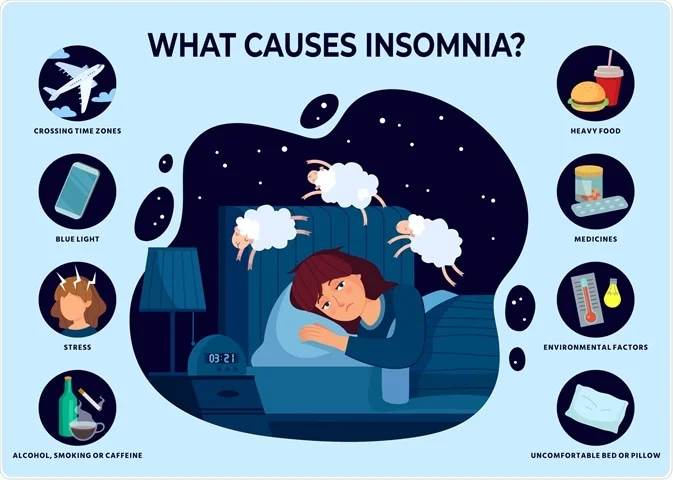
Causes and Risk Factors:
- Stress and anxiety
- Irregular sleep schedule
- Poor sleep environment
- Stimulants (caffeine, nicotine)
- Electronic screen use before bedtime
- Medical conditions (pain, sleep apnea)
- Medications
- Lifestyle factors (shift work, travel)
Consequences:
- Impaired cognitive function
- Mood disturbances (depression, anxiety)
- Increased risk of accidents and injuries
- Reduced productivity and performance
- Weakened immune system
- Cardiovascular disease
Diagnosis:
- Clinical evaluation
- Sleep diary or actigraphy
- Polysomnography (PSG)
- Diagnostic criteria (DSM-5 or ICSD-3)
Treatment Options:
- Cognitive Behavioral Therapy for Insomnia (CBT-I)
- Sleep hygiene practices
- Relaxation techniques (progressive muscle relaxation, mindfulness)
- Stimulus control therapy
- Medications (sedatives, hypnotics)
- Lifestyle modifications (regular exercise, sleep schedule)
Lifestyle Changes:
- Establish consistent sleep schedule
- Create sleep-conducive environment
- Avoid screens before bedtime
- Limit caffeine and nicotine
- Engage in relaxing activities before sleep
- Regular physical activity
